| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B2229breast 髓样癌, yes or no?(cqz-26) 9-1-2009
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
-
本帖最后由 于 2009-09-26 08:24:00 编辑
相关帖子
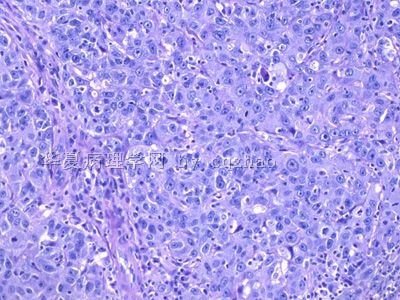
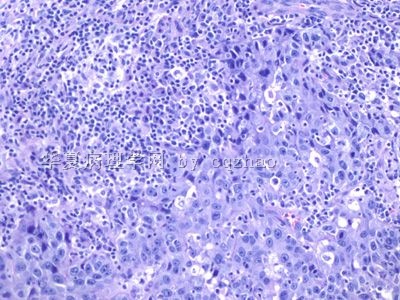
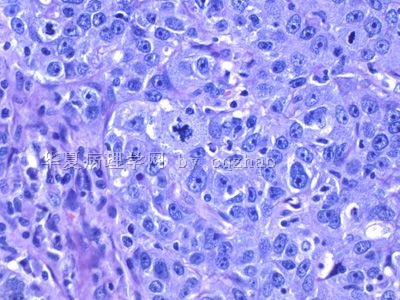
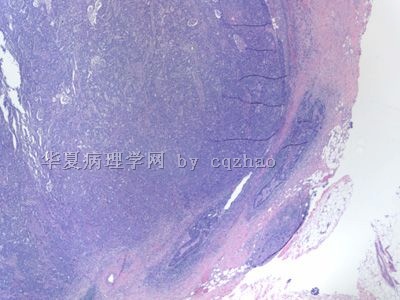
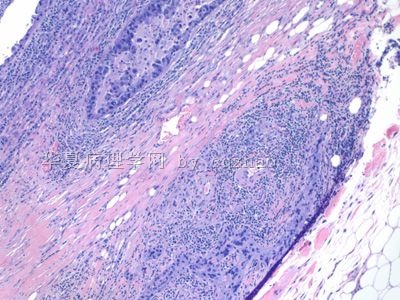
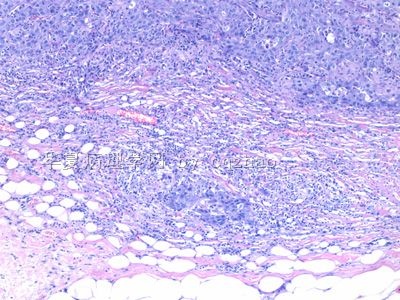
This is one of my today's large breast cases. Aged about 59 y women with breast tumor mass measuring 3 cm, grossly with demarcated margins. Clearly it is a high grade carcinoma with a lot of lymphocyte infiltrates. Most areas of the margins are like fig 1 and 2, very focal areas like the last three photos.
Just wonder what should we call for this case. No IHC needed.
Thanks, cz
Dr.Zhao,
It's very nice to learn your cases. Many thanks!
I think this is case of medullary carcinoma.
Syncytial growth pattern, absence of glandular structure,lymphocyte infiltrate, moderate nuclear pleomorphism and well circumscribed, all features support medullary carcinoma.
WHO 2003 关于髓样癌有5个诊断特征,本例都符合。
典型的MC具备五大形态特征:
1、在超过75%的肿瘤范围内可见到合胞体结构。肿瘤细胞片状排列,常超过4或5个细胞的厚度,被少量疏松结缔组织隔开,可见局灶坏死和鳞状分化。
2、极少有腺样或小管结构。
3、间质内弥漫性淋巴浆细胞浸润是其明显特征,浸润程度各不相同。单核细胞少见或多得以至于把肿瘤细胞都掩盖了。可见淋巴样滤泡和/或上皮样肉芽肿。
4、肿瘤细胞通常为圆形,胞浆丰富,泡状核,核仁1个或几个,胞核中等异型或异型显著,核分裂象多见,可见到不典型巨细胞。
5、低倍镜下可见到肿瘤完整的包膜,在肿瘤周围形成压排性边缘与被压迫的纤维间质区相互混合。
一些学者提出了被其他人接受的观点,即除这些典型的组织学特征外,导管内成分的存在也可作为一条排除其它诊断的标准,特别是位于肿瘤周边组织或在肿瘤内缩至小范围的区域。
这些诊断标准,特别是肿瘤边缘情况,在实际中很难估计,这也可以解释在一些研究中MC诊断低重复性的原因。为了克服困难,人们又提出了一个简化的标准,即合胞体样生长方式、小管结构缺乏、淋巴浆细胞浸润及少量的坏死。这些被认为是MC最具重复性的特征,但是这一简化标准的有关预后的意义尚待评价。具有明显的合胞体结构但只具有其它2条或3条特征的MC通常被诊断为不典型髓样癌(AMC)。

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
| 以下是引用Elizabeth在2009-9-4 8:36:00的发言:
Dr.Zhao, It's very nice to learn your cases. Many thanks! I think this is case of medullary carcinoma. Syncytial growth pattern, absence of glandular structure,lymphocyte infiltrate, moderate nuclear pleomorphism and well circumscribed, all features support medullary carcinoma. |
| 以下是引用cqzhao在2009-9-5 1:22:00的发言:
Interesting. Most of people would sign out as 髓样癌. Questions: How often did you sign out 髓样癌 in your daily work? If you have 100 breast ca, how many cases are diagnosed as 髓样癌by you or your colleaques? |

- 博学之,审问之,慎思之,明辨之,笃行之。
-
本帖最后由 于 2009-09-06 20:09:00 编辑
-
Find some original paper abstrats about classification systems for medullary carcinoma (MA). They are similar, but with some difference. I am pasting some paper abstracts for some ones who have good English and are interested to this area.
Cancer. 1977 Oct;40(4):1365-85.
Medullary carcinoma of the breast: a clinicopathologic study with 10 year follow-up.
-
Hum Pathol. 1988 Nov;19(11):1340-6.
-
Medullary carcinoma of the breast: a clinicopathologic study with appraisal of current diagnostic criteria.
Department of Pathology, George Washington University Medical Center, Washington, DC 20037.
Fifty-three cases of mammary carcinoma originally diagnosed as medullary carcinoma (MC) or infiltrating duct carcinoma (IDC) with medullary features were reviewed and reclassified using the strictly defined histologic criteria applied a decade ago by Ridolfi et al. Our study interval (1961 to 1982) allowed for a minimum follow-up of 5 years for each patient, with a mean follow-up period of 7.2 years. When reclassified, 24 tumors fulfilled the criteria for MC, 16 tumors were determined to be atypical MC, and ten tumors were found to be IDC; the observed 5-year survival rates were 95%, 80%, and 70%, respectively. These findings confirmed those of other investigators, that when specific criteria are applied, MC proves to be a form of mammary carcinoma with a favorable prognosis. However, we also found that when tumors were excluded from the MC category solely on the basis of in situ carcinoma, focal marginal infiltration, or a sparse mononuclear infiltrate, the survival rate of these patients was similar to that of patients in the medullary category. Thus, we propose that one of these criteria alone should not suffice to exclude the diagnosis of MC. On the other hand, tumors with two or more of these atypical features, or with extensive marginal infiltration, no mononuclear cellular infiltrate, and/or less than 75% syncytial growth, should be classified as IDC with medullary features. Typical MC with bland nuclei or a focal microglandular growth pattern only were not observed in this series; however, these findings should probably also cause a tumor to be classified in the IDC category. By dividing our cases into two rather than three groups, we found a statistically significant difference between the survival rates of 94% and 64% for MC (34 tumors) and IDC (14 tumors), respectively. Although the latter figure probably exceeds the survival rate for IDC without medullary features, the difference does not appear great enough to warrant a separate diagnostic category.